Dementia and driving: Families, doctors wrestle with when to take away keys

Nancy Urban knew all the back roads in Suffolk. She used to chauffeur her three young girls all over town. And when they needed directions as adults, she had all the shortcuts.
So when Urban got lost driving to Patchogue in 2015, alarm bells went off for her daughter Stephanie Garcia.
Urban, then 55, called Garcia for help. “She knew that area well. I couldn't believe she didn't know where she was,” Garcia said. She slowly guided her mom to a highway and later learned it wasn't her first driving mishap.
Days after that episode, Garcia noticed her mother couldn't shift her Ford Focus into reverse. Family suggested Urban stop driving, but she wouldn't completely give it up until months later. And that was only after she received a new medical diagnosis of early-onset Alzheimer's, a type of dementia that develops in people under 65.
WHAT TO KNOW
Deciding when patients with dementia should hang up the car keys does not have a one-size fits-all approach, experts said.
It’s often a gut-wrenching ordeal for families and patients.
Experts said it will remain an ongoing concern as dementia cases continue to grow.
Urban's ordeal highlights a difficult decision faced by families and doctors: when to stop those with dementia from driving. Experts said the issue will continue to grow as the number of people with Alzheimer's is expected to double nationwide by 2050. More than 6 million people are currently living with Alzheimer's in the United States, according to the Alzheimer's Association.
Families and experts said knowing precisely when a person battling early or mild stages of dementia should give up the keys is complicated. The disease develops and progresses at different rates, making the decision highly personalized, according to medical experts. A person’s independence must be balanced with safety. Health professionals and families don't want to stop someone from driving prematurely or wait too long until it's potentially dangerous for themselves or others.
“It's one of the many, deeply personal challenges of dementia,” said Dr. Alan Mazurek, assistant clinical professor of neurology at Mount Sinai Hospital in New York City and chairman of the Medical Advisory Council at the Alzheimer’s Association on Long Island. “Driving is especially difficult and challenging in suburban areas like Long Island where transportation is so dependent on car travel.”
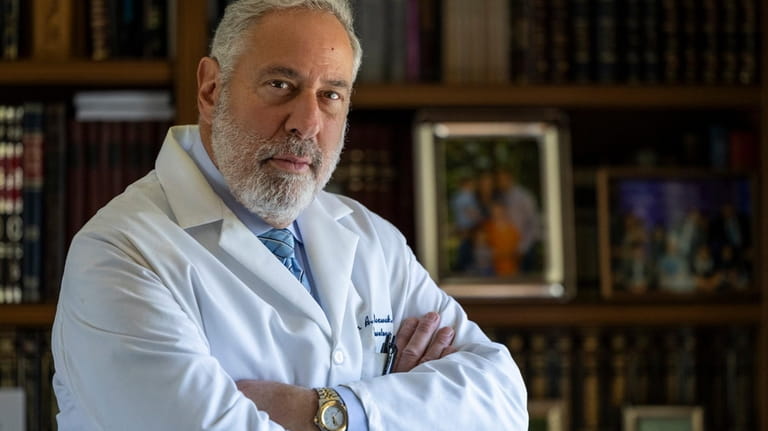
The decision to stop driving is a "communal process" between doctors, patients and family members, said Dr. Alan Mazurek, chairman of the Medical Advisory Council at the Alzheimer's Association on Long Island. Credit: Corey Sipkin
In some states, a dementia diagnosis requires doctors and health professionals to alert their motor vehicle or health departments. New York has no such mandate.
Instead, Mazurek called the decision a “communal process,” made between doctors, the patient and family members.
“It's hard to give blanket policies when somebody has some difficulty because every case is really unique to itself,” he said.
Studies have found that while drivers with dementia are at increased risk of crashing, most patients in the early stages of the condition can continue driving safely.
“It's very complicated because where do we draw the line? It's very tough to make those decisions,” said Dr. Allison B. Reiss, associate professor of medicine at NYU Long Island School of Medicine.
“No matter what, at some point you can't drive, but how long does it take and what are the manifestations and the symptoms and the order of the symptoms?” said Reiss, who is also on the Alzheimer’s Foundation of America’s Medical, Scientific and Memory Screening Advisory Board.
Dementia signs not always evident
While families acknowledged the medical condition might pose safety risks on the road, they also said the signs might not be evident until it's too late.
Before Urban's Alzheimer's diagnosis, her mental lapses were misdiagnosed and attributed to her multiple sclerosis. With no guidance from doctors, her husband tried to discourage her from driving, but his efforts weren't enough.
Nancy Urban next to her 1983 Oldsmobile Cutlass in the 1990s. Urban knew all the back roads in Suffolk and when her three daughters needed directions, she had all the shortcuts. Credit: Newsday/John Paraskevas
“I had to go to several doctors because they didn’t want to believe it,” said Garcia. “She was exhibiting memory loss for two years and they were giving her memory games on her laptop and they kept trying to link it to her multiple sclerosis.”
Once a doctor broke the news of her new diagnosis and confirmed she could no longer drive, the family got on same page, Garcia said. It wasn't easy for Urban, but she took the news in relative stride, believing it would be a temporary break.
“My mom would get upset and cry … it was constant redirecting,” said Garcia, of Islip Terrace. “We had to start finagling how we could trick mom into not driving ever again.”

Nancy Urban, right, with her husband Glen, center, at Spirit's Promise Equine Rescue Farm in Riverhead in 2017. Credit: Newsday/Alejandra Villa
The family moved her car from the front of her house because it was a constant trigger, later selling it to a college student. This eased the transition for Urban, who died in 2020.
Dr. Nikhil Palekar, director of the Center of Excellence for Alzheimer’s Disease and Division of Geriatric Psychiatry at Stony Brook University Hospital, said he has seen patients being told they can no longer drive go through the five stages of grief.
“First there is denial … They say, 'I’m fine, there are no issues.' Then there is a bargaining. Then we say, 'No, that’s not safe,' and then there is anger. They may lash out toward me verbally or toward the family and say it’s not fair and then they feel a sense of hopelessness and then ultimately acceptance,” Palekar said.
Driving involves a complex skill set, including focus, attention, the ability to estimate space, speed and distance, and fast reaction time. Dementia impacts cognitive and motor skills, and as it progresses may affect driving by reducing spatial awareness and slowing response times, leading to difficulty with directions and following traffic signals, medical experts said.
Neurologists or geriatric doctors will first talk to the patient, their families and caregivers about whether there have been any collisions or near crashes, whether they’re getting lost or whether their reaction time is delayed. Families are also routinely asked whether they would feel safe having their grandchildren in the car with them. Doctors may also conduct a cognitive screening. If the prognosis is still murky, they will recommend the patient take an on-road driving test at a driving school. If the patient passes the driving evaluation, doctors may still recommend restrictions.
In early stages of dementia, doctors may recommend patients only drive locally on familiar roads because patients will suffer short-term memory loss before long-term memory is impacted, Palekar said. He might also advise patients to only drive during the day, because there would be an added disadvantage of not seeing clearly at night.
“It’s not a one size fits all model, so you have to really evaluate patients at where they’re at,” he said.
No NYS reporting mandate
While the state has no mandate for health professionals to report dementia diagnosis, if a police officer, doctor, or any individual is concerned about someone’s ability to drive, they can request a driver re-evaluation at the DMV by filling out a form.
After reviewing the form, a license examiner from the DMV might require the driver come in for an interview, plus take a written and a driving skills test. The driver might also be asked to bring a physician statement clearing them to drive. If a doctor does not find the person is medically fit to drive, the DMV will suspend the driver's license.
Last year, the DMV received 3,047 requests for driver re-evaluations for a variety of reasons from police officers, physicians or concerned citizens, according to Tim O'Brien, spokesman for the agency.
According to the Alzheimer's Association Long Island Chapter, an estimated 410,000 people were living with Alzheimer’s in New York and over 60,000 on Long Island last year. New York has the second-highest Alzheimer’s rate of all states, Newsday previously reported. Nassau County ranked 7th of 62 counties with a prevalence rate of 12.5% of people 65 and over while Suffolk ranked 11th of 62 counties with a prevalence rate of 11.7%, according to a 2023 study showed.
Experts said not being able to drive not only represents a major loss of autonomy for dementia patients, it can also be isolating if alternative travel options aren't in place.
Several Long Island doctors said in interviews that in most cases they believed there is no need to report dementia to government officials because they felt additional government oversight wouldn't prevent a patient who lacks comprehension from getting behind a wheel. It may also strain the doctor-patient relationship by deterring people from opening up about their symptoms, and they said most patients comply with the doctor's guidance.
The American Medical Association said in an email it has no position “on mandated reporting of a dementia diagnosis to a motor vehicle licensing authority.”
Dr. Mariel Deutsch, the founder of Neurology Mind Care in Merrick, trained in California, where doctors are required to report dementia patients to the health department which then notifies transportation officials. She found it to be harsh and often distracting for patients.
“In a reporting state, sometimes it ends up being just the focus on the act of reporting itself. That is kind of troublesome,” said Deutsch, who is holding a free webinar March 20 about dementia and driving for health care professionals and caregivers.
She said it's important for patients to feel they're in a supportive and therapeutic environment where they can discuss their symptoms without fear.
But Tori Cohen, executive director at Long Island Alzheimer's & Dementia Center in Westbury, said because dementia is a progressive disease, mandatory reporting could help families, and also help track crashes linked to dementia. The DMV does not currently track crashes associated with dementia.
“I do think that when someone gets a diagnosis that it needs to be reported,” Cohen said, adding that symptoms of dementia can rapidly evolve. “I think it's preventive because you're trying to save lives because there are people that shouldn't even be driving to begin with who are on the road right now.”
She noted it's not just an older person's disease, but is “affecting younger people as well.”
Hiding keys, disconnecting batteries: caregivers' creative techniques
Mike Henley, of Westbury, was 36 years old when he was diagnosed with Familial Alzheimer’s disease in April 2001. His widow, Karen Henley, didn't wait for a doctor's recommendation to take her husband's keys. She had noticed his driving abilities had been slipping and he got lost returning from a psychiatrist’s appointment several months before the diagnosis. While it was emotional for him, he didn't fight the decision.
“I wasn’t going to put myself or the family in any situation where he would hurt himself or somebody else,” Karen Henley said of her husband, who died in 2012. “There were a lot of tears.” They eventually donated the car to a veterans' group.
Driving on Long Island is often necessary to get to medical appointments, pharmacies and supermarkets. That's why experts said it's important for families to talk about transportation alternatives early, even when driving does not appear compromised. If a person must stop driving but refuses to, family should not get confrontational.
“We always talk about appealing to their sense of responsibility for the greater good,” said Taryn Kutujian, senior community education manager at the Alzheimer's Association Long Island Chapter.
Caregivers may resort to creative techniques like hiding keys, disabling the car, or simply moving the car and selling or donating it.
Some families go to great lengths to keep their relatives from getting behind the wheel.
Laura LaFauci, Long Island director of community outreach at Amber Court Communities and chair of the Westbury-based National Aging in Place Council, said that stopping her strong-willed grandfather, Max Fleischman, of West Babylon, from driving after his dementia diagnosis in 2013 was difficult. LaFauci said family began dissuading him from driving in 2011 after noticing his car would come back with mysterious scuffs and broken mirrors, but Fleischman, an Army veteran, would not give up so easily. His doctor told him that as long as he could see, he could drive.
LaFauci said that in 2013, the family took matters into their own hands, disconnecting the car’s battery. He then walked around the corner and bought himself a new one. They later moved the car and told him it was stolen.
“The last straw was he hit something with the car and we still don’t know what he hit and that’s when we decided to take it,” LaFauci said.
Even after that, Fleischman managed to get to a car dealership and attempted to buy another vehicle, but LaFauci was able to intervene.
LaFauci said a mandate would have been helpful in her grandfather’s case because the primary care doctor he was seeing did not feel his skills were impaired.
“I would love to see more legislation and I think that physicians should have to report it,” LaFauci said.
Adding to the complex issue of when to stop driving is the challenge of getting a formal dementia diagnosis.
Palekar said some primary care doctors may simply link an elderly patient’s concern about being forgetful to the natural aging process, but he said that the Center of Excellence for Alzheimer’s Disease is educating the community about signs of the condition while also giving primary care physicians the tools to take patients' concern one step further. He said there are simple tests that check for cognitive issues, and patients who test positive should get referred to a specialist.
With or without a dementia diagnosis, some families feel the driving decision should reside with the individual and their loved ones.
David Tobachnik, of Coram, said that in 2013, his father, Edgar Tobachnik, was ordered by police to take a road test after his foot slipped off the brake pedal and he bumped into a pole. Edgar passed the test, but not before his family took him to a hospital where he also passed a cognitive screening.
Two years later, in declining health, he stopped driving at his family's urging. With his senses no longer as sharp, they emphasized how a delayed reaction time could cost someone's life.
David supports more frequent driver evaluations in New York, but not mandatory reporting.
“We felt it was very important for his self esteem to be a participant in when to stop driving,” said David, a private pilot. “I think it would have been devastating for the state to say you can’t drive anymore.”
What to do if you’re concerned that someone’s driving skills are impaired by dementia
- Do not wait to have a conversation. Tell them you're concerned about their well-being and afraid they or someone else can get hurt. Don't assume someone with dementia has no comprehension. Be kind, supportive and understanding.
- Have a transportation plan in place early. This could mean having family help, hiring outside help, using taxis or app-based rides, or, when possible, finding accessible public transit. Get deliveries when possible.
- Seek medical help, including a diagnosis and a health professional’s recommendation.
- Get a driving evaluation at a driving school with a specialist.
- If the person is resistant to giving up the keys, do not become confrontational. Remove access to the car, either by disabling it, moving it, selling or donating it.
- Find support services from groups like the Alzheimer’s Association or Long Island Alzheimer's and Dementia Center.
- Build a network outside your family. Do not be afraid to reach out to your community or local house of worship.
Warning signs that someone’s driving is impaired
- Mysterious dents on the car
- Minor or major crashes
- Forgetting places and getting lost
- Difficulty following traffic signals and patterns
- Driving too slow or fast
- Delayed reactions
Sources: Compiled by Newsday from Alzheimer's Association, Long Island Alzheimer's & Dementia Center, doctors and advocates.
